Chronic Obstructive Pulmonary Disease (COPD)
By Megan Hodgson
Reviewed by YardCard Team (Dr N Gittens - SHO)
What is COPD?
Chronic Obstructive Pulmonary Disease (COPD) is a preventable and treatable disease characterised by non-reversible, progressive airflow obstruction.
It is caused by inflammatory damage to lung tissue (e.g. from tobacco smoking). This makes the lungs harder to ventilate and more vulnerable to infection.
COPD is a combination of 2 conditions:
- Chronic Bronchitis - chronic inflammation of the mucous membranes in the bronchioles, causing bronchospasm, excess mucus hypersecretion & productive cough
- Emphysema - damage/breakdown to the alveolar wall, causing enlargement of the distal airspaces, forming bullae
Diagnosis of COPD is based on clinical features and is supported by spirometry.
Patient-centred explanation
"Chronic obstructive pulmonary disease (COPD) is the name for a group of conditions where air cannot get out of the lungs easily. It includes emphysema (damage to the air sacs in the lungs) and chronic bronchitis (long term inflammation in the airways). It's common in middle-aged or older adults who have smoked, as well as people who've had occupational exposure to fumes. The damage to the lungs is permanent, but treatment can slow down progression. The most important treatment is stopping smoking if you have not stopped already."
Pathophysiology
Chronic Bronchitis
- Chronic bronchitis is characterised by hypersecretion of mucus by Goblet cells in the bronchi & bronchioles of the lungs as a protective reaction to exposure to smoke or other pollutants. The cilia cannot remove the excess mucus, causing obstruction of the small airways
- Ongoing inflammation causes remodelling & thickening of the airway walls, worsening the airway obstruction

Emphysema
- Lung inflammation is facilitated by excess protease activity. This inflammation is counter-acted by protease inhibitors (antiproteases), e.g. alpha-1 antitrypsin
- Smoke & other pollutants reduce the activity of antiproteases (e.g. alpha-1 antitrypsin)
- Without sufficient antiprotease activity, proteolytic enzymes produced by inflammatory cells break down the alveoli walls. This causes enlargement of the terminal airspaces and reduces the surface area available for gas exchange

Risk Factors
Modifiable (Environmental) Risk Factors
- Cigarette smoking - 90% of cases
- Passive cigarette smoke exposure
- Marijuana smoking
- Occupational exposure (e.g. asbestos, dust, fumes)
- Household air pollution (e.g. wood or coal burning)
Non-modifiable Risk Factors
- Older Age
- Alpha-1 antitrypsin deficiency
- Air pollution
- Asthma
Signs & Symptoms
Symptoms
- Productive cough
- Chronic, progressive dyspnoea
- Chest tightness
Signs
- Expiratory wheeze
- Decreased cricosternal distance (secondary to hyperinflation)
- Barrel chest (secondary to hyperinflation)
- Use of accessory muscles
- Pursed lip breathing (creates positive end expiratory pressure to prevent alveoli collapse)
- Symptoms of right-sided heart failure (cor pulmonale): peripheral oedema, raised JVP
- Cyanosis
- Cachexia
Breathlessness can be assessed according to the mMRC breathlessness scale:
mMRC Dyspnea Scale| Please tick in the box that applies to you (one box only) | ||
|---|---|---|
| mMRC Grade 0 | I only get breathless with strenuous exercise. | |
| mMRC Grade 1 | I get short of breath when hurrying on the level or walking up a slight hill. | |
| mMRC Grade 2 | I walk slower than people of the same age on the level because of breathlessness, or I have to stop for breath when walking on my own pace on the level. | |
| mMRC Grade 3 | I stop for breath after walking about 100 meters or after a few minutes on the level. | |
| mMRC Grade 4 | I am too breathless to leave the house or I am breathless when dressing or undressing. | |
Symptoms severity can be assessed using the CAT (COPD Assessment Test)

Investigations
Spirometry
- Spirometry is used to measure pulmonary function (e.g. lung capacities & the rate of air flow in and out of the lungs)
- This is the definitive investigation to confirm the diagnosis of COPD & is used to monitor progression of disease
- After the initial spirometry reading, spirometry is repeated 15-20 minutes after taking a short-acting bronchodilator (post-bronchodilator spirometry)
- Finding: Obstructive respiratory disease (post-bronchodilator FEV1/FVC < 70%). A post bronchodilator FEV1/FVC less than 0.7 confirms persistent airflow obstruction.
Staging of COPD - GOLD Classification of COPD Severity
| Severity Classification | Post-Bronchodilator FEV1/FVC | FEV1 (% of predicted) |
|---|---|---|
| Mild (Stage 1) | <0.7 | >80% |
| Moderate (Stage 2) | <0.7 | 50-79% |
| Severe (Stage 3) | <0.7 | 30-49% |
| Very Severe (Stage 4) | <0.7 | <30% |
Other Investigations
- Chest X Ray: to exclude other causes of the clinical syndrome
- FBC: to look for any abnormalities such as anaemia or polycythaemia
- Alpha-1 antitrypsin: can αe considered if deficiency is suspected. a-1-antitrypsin deficiency is more likely in people with early onset of symptoms, minimal smoking history or a family history of this condition.
- ECG, BNP, Echo: can be considered if pulmonary hypertension or cardiac disease are suspected
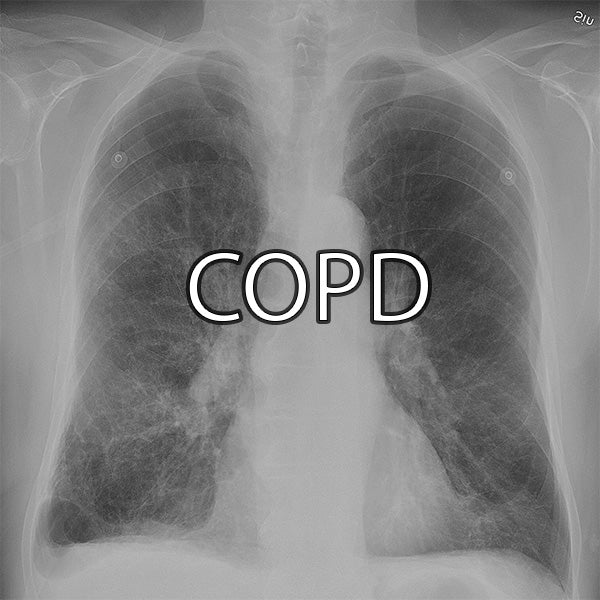
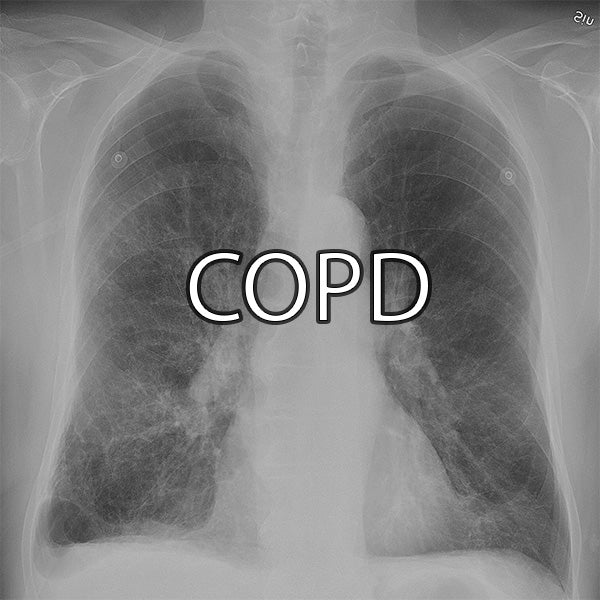
Chest X-Ray
- Findings:
- Hyperinflation (>8 anterior ribs visible)
- Flattened hemidiaphragm
- Bullae
- Reduced lung markings
- Prominent hila
- Used to exclude other causes (e.g. lung cancer, bronchiectasis, tuberculosis & heart failure)
Bloods: FBC
- Finding: Secondary polycythaemia (from chronic hypoxaemia)
ECG
-
Findings: Changes in advanced COPD with Cor pulmonale
- Right axis deviation
- Prominent P waves in inferior leads
- P pulmonale
- Right ventricular strain pattern
- Right Bundle Branch Block (RBBB)
Management
Conservative Management
• Smoking cessation - offer nicotine replacement therapy.
• One-off Pneumococcal vaccine
• Annual flu vaccine
• Pulmonary rehabilitation (MRC grade 3 or above)
• Referral to Respiratory Physiotherapy (to help with sputum clearance and breathing techniques)
Stepwise Medical Management
• STEP 1: Short-acting bronchodilators (SABA/SAMA)
• Beta-2 agonists (e.g., salbutamol or terbutaline) - SABA
• Antimuscarinics (e.g., ipratropium bromide) - SAMA
• STEP 2: Assess for Asthmatic/steroid responsive features
• Asthma or atopy diagnosis
• High serum Eosinophil count
• Substantial variation in FEV1 over time (>400ml)
• Substantial diurnal variation in peak expiratory flow (>20%)
• STEP 3 (no steroid-responsive features): SABA + LABA + LAMA
• Long-acting bronchodilators (e.g., salmeterol and formoterol) - LABA
• Long-acting muscarinic antagonists (e.g., glycopyrrolate or tiotropium) - LAMA
• STEP 3 (steroid-responsive features): SABA/SAMA + LABA + ICS (Inhaled corticosteroids)
• Inhaled corticosteroids (e.g., beclomethasone, budesonide) - ICS
• STEP 4: SABA + LABA + LAMA + ICS
Other Medical Management
Oral Theophylline
Used after trials of short & long-acting bronchodilators OR those intolerant to inhaled therapy
Oral Prophylactic antibiotic therapy
Azithromycin 500mg three times per week
Indications: non-smokers, optimised treatment & continued exacerbations (>3 exacerbations requiring steroids or ≥1 exacerbation requiring hospital admission in the last year)
CT thorax & Sputum culture required before prescription of prophylactic antibiotics in COPD to exclude bronchiectasis, atypical infections & tuberculosis
Mucolytics
e.g. Carbocystine
Considered in stable COPD patients with a chronic productive cough where mucolytic improves their symptoms
Nebulisers
Considered in patients with disabling breathlessness despite optimised use of inhalers
Long-term Oxygen Therapy (LTOT)
After smoking cessation, LTOT is one of few interventions shown to improve survival in COPD
Oxygen is used for at least 15 hours per day. Ensure patients are medically optimised & COPD is stable (i.e. not recovering from a recent exacerbation)
Contraindication: Smoking (risk of burns & fire)
LTOT should be offered to:
- Patients with a pO2 of <7.3 kPa (on 2+ ABGs 3 weeks apart)
- Patients with a pO2 of 7.3 - 8 kPa (on 2+ ABGs 3 weeks apart) and 1 of the following:
- Secondary polycythaemia
- Pulmonary hypertension
- Nocturnal hypoxaemia
- Peripheral oedema
References
- BMJ Best Practice. 2024. Chronic Obstructive Pulmonary Disease (COPD). Available at: https://bestpractice.bmj.com/topics/en-gb/7 [Accessed 23 October 2024].
- Chronic obstructive pulmonary disease. Available at: https://cks.nice.org.uk/topics/chronic-obstructive-pulmonary-disease/ [Accessed 23 October 2024].
Image Credits
- https://commons.wikimedia.org/wiki/File:Bronchitis.jpg via Wikimedia Commons
- https://commons.wikimedia.org/wiki/File:Copd_2010Side.JPG via Wikimedia Commons
- https://www.tandfonline.com/doi/full/10.2147/COPD.S62750 via Wikimedia Commons





Leave a comment